Breakthrough Protein Unlocks Body’s Healing Power for Spinal Injuries

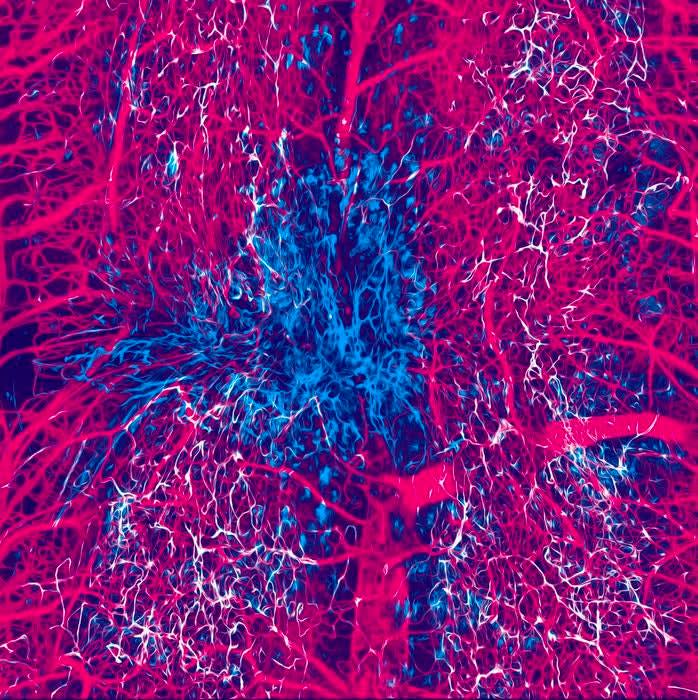
At the core of your body's healing mechanism lie minute cells possessing great strength—pericytes. These compact yet energetic cells encircle the tiniest blood vessels and assist in maintaining and repairing tissues. Recently, innovative studies suggest that pericytes could pave the way for a future where injured spinal cords have the potential to regenerate, both physically and in terms of functionality. For many years, researchers debated whether pericytes aided or hindered recovery following spinal cord damage. However, there is now a more definitive response—and it offers optimism.
From Problem to Possibility
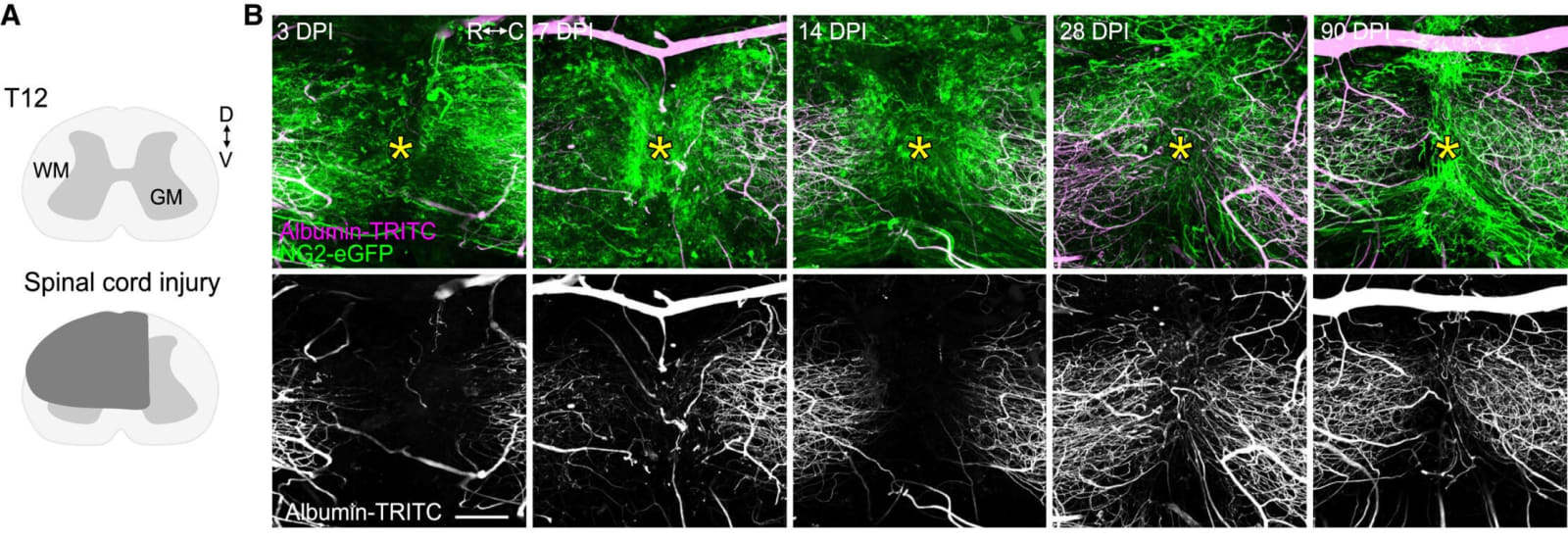
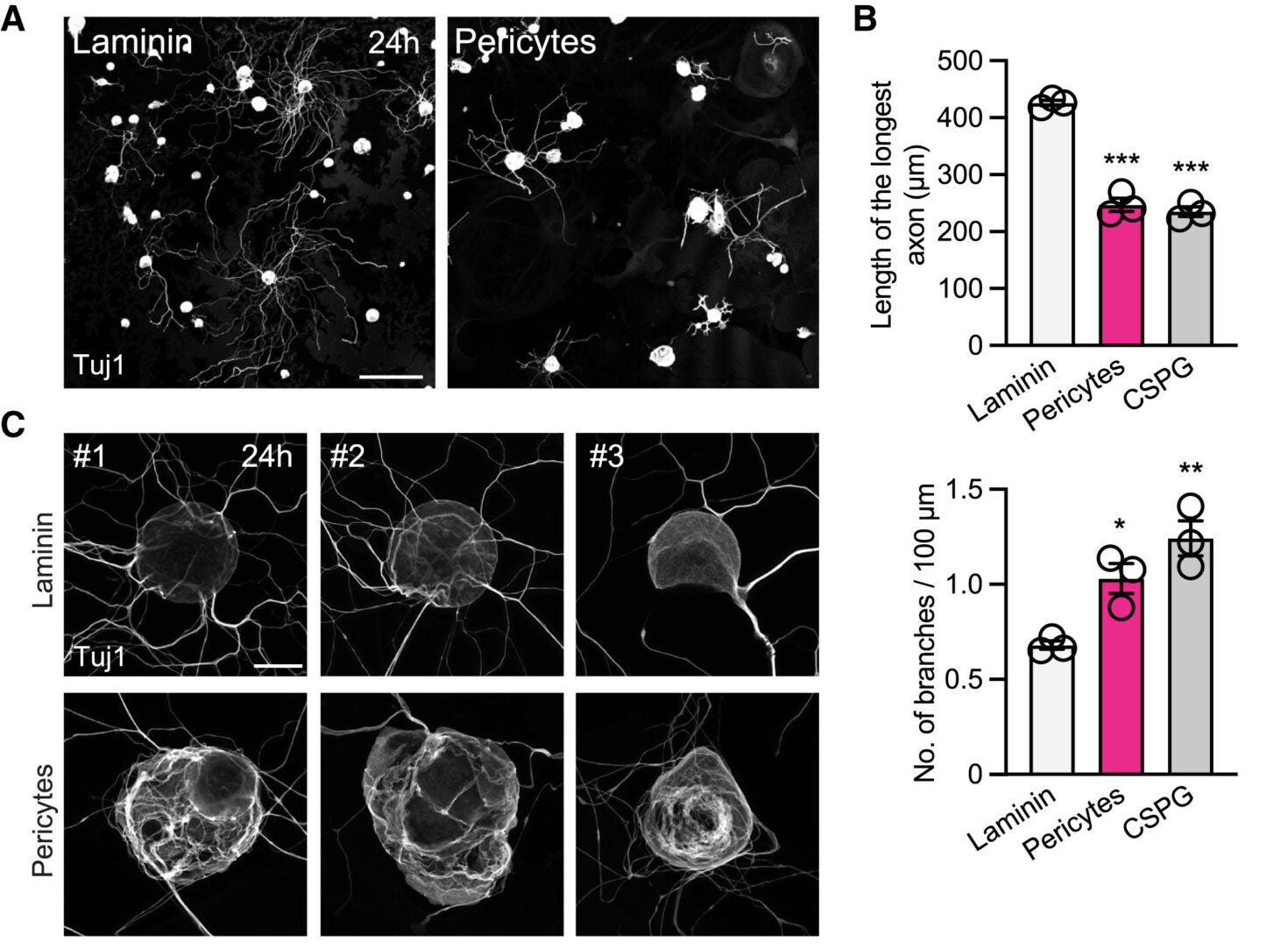
After a spinal cord Injury causes multiple system failures—not only involving nerves. Blood vessel function ceases, inflammation expands, and regular cell movement stops. Among the initial group of cells to reach the injury site are pericytes. These cells move toward the affected region, yet rather than aiding recovery, they can contribute to issues. Researchers observed that pericytes strongly adhere to sensory axons—the elongated sections of nerve cells responsible for transmitting signals throughout the body. This interaction interferes with the axons, complicating their ability to regenerate.
But what if these identical pericytes were transformed into allies rather than obstacles?
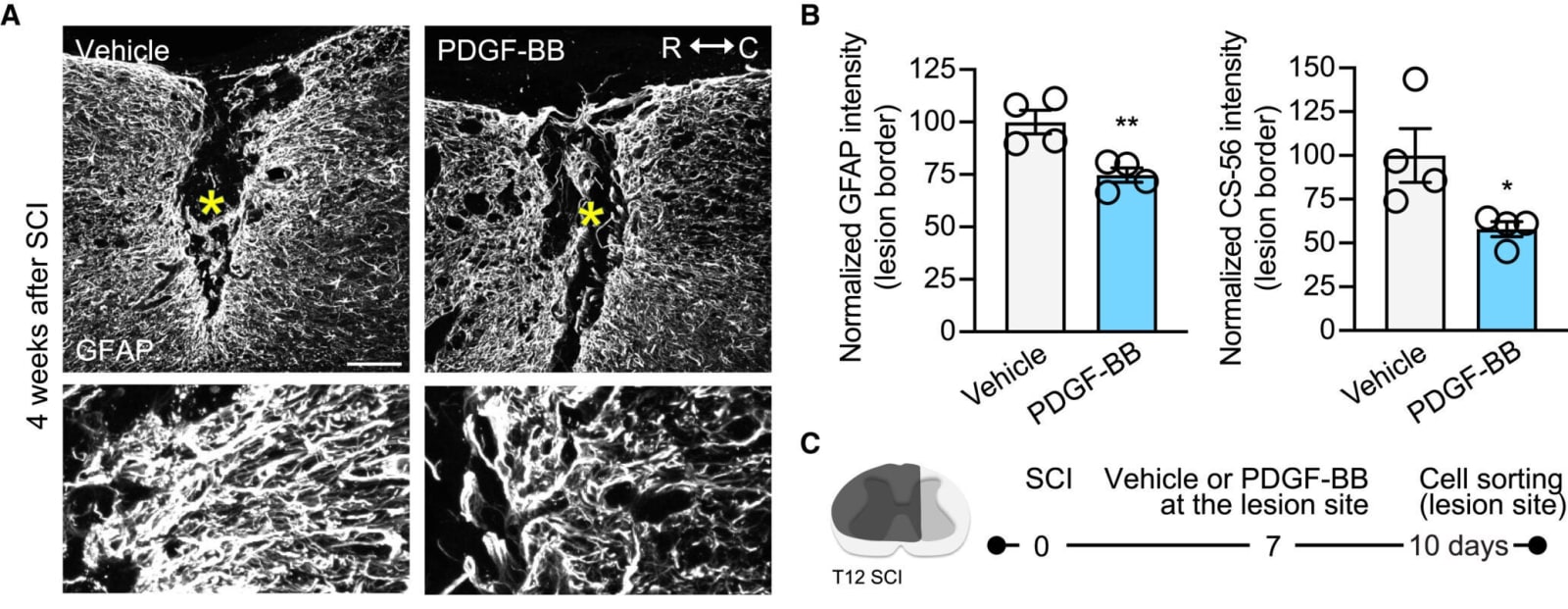
Researchers from Ohio State University discovered a method to change their position. By administering a single injection of a protein known as PDGF-BB (platelet-derived growth factor BB), they managed to alter the pericytes near the damaged area. After being exposed to PDGF-BB, the cells changed their shape and exhibited new behaviors. They ceased making certain substances and instead released different ones that promoted the regrowth of axons.
There's much yet to discover and many areas for growth," stated Andrea Tedeschi, lead researcher and neuroscience professor. "However, as we delved deeper into this work, we became increasingly amazed by the strength of this one treatment and just how successful it proved to be.
Building Cellular Bridges
One of the most impressive discoveries involved how pericytes responded following PDGF-BB administration. Typically, these cells gather at the site of injury but do not form functional structures. blood vessels or design a route for nerve cells to travel along.
Related Stories
・ A flexible electronic gadget encircles the spine — transforming the approach to treating spinal damage
・ A gel made from cow mucus might transform the treatment of spinal cord injuries.
・ A groundbreaking deep brain stimulation treatment helps regain mobility following a spinal cord injury.
After treatment, pericytes altered their form — becoming elongated and narrow — and began creating structures known as "cellular bridges" by scientists. These connections served as physical routes that facilitated the growth of axons.
In experiments with mice, scientists administered PDGF-BB directly into the injured spinal cord seven days post-injury—an interval comparable to a nine-month recovery period in people. After four weeks, axons were much larger in mice receiving the treatment compared to those that did not. These nerve fibers seemed to utilize the bridges formed by pericytes to bypass the injured area.
When examining the formation of these pericyte structures spanning the injury area, we observed that the treatment encouraged the development of these connections," said lead researcher Wenjing Sun. "Nearly all, if not all, of the regenerating axons managed to bypass the injury site by utilizing these cellular bridges.
These structures not only supported axon growth, but the mice also recovered mobility in their hind legs. Electrophysiological tests indicated that signals were able to pass through the injured region. The treated animals performed more effectively in motor assessments and exhibited less evidence of... nerve pain a frequent and challenging consequence of spinal cord injuries.

Healing More Than Nerves
This therapy had effects that extended past aiding nerve regeneration. The protein PDGF-BB also played a role in rebuilding small blood vessels. This is significant since, following an injury, the interruption of blood circulation prevents oxygen and essential nutrients from reaching the cells working to mend the harm. Restoring these blood vessels allowed the scientists to establish a better environment for healing.
Subsequent investigation revealed that pericytes did not transform into different types of cells following treatment. They maintained their initial structure but assumed additional roles. Although certain genes associated with conventional pericyte functions decreased in activity, others involved in the repair process became more active.
A reduction was observed in certain traditional pericyte indicators, yet an increase in new functions associated with efforts to restore cell connections and functional blood vessels," Sun stated. "Based on the general genetic profile from our findings, they are still categorized as pericytes.
The treated region also showed reduced instances of inflammation which typically leads to greater harm following spinal cord injuries. This additional advantage probably contributed to decreased pain in the mice and facilitated improved long-term recovery.
From Mouse to Human Promise
Even though this study started with mice, the researchers made efforts to determine its applicability in humans. In laboratory tests, they utilized human pericytes and subjected them to PDGF-BB, after which they implanted mouse cells. neurons above. The outcome was similar to what occurred in the mouse models, with axons beginning to grow quickly.
To enhance the clinical significance of our results, we grew mouse nerve cells over human pericytes that had been treated with PDGF-BB," stated Tedeschi. "This proved enough to induce a growth-enhancing response, indicating that this could indeed be a broad-based process not limited to mice.
This creates an opportunity for upcoming therapies beyond spinal cord injuries as well as for brain injuries injuries, strokes, and conditions where nerve growth is delayed or halted. As PDGF-BB influences the surroundings of the damage rather than solely the neurons, it could potentially be combined with other medications that specifically target nerve cells.
One example of this medication is gabapentin, which Tedeschi and Sun previously investigated. It functions by improving the capacity of nerve cells to grow. When used alongside PDGF-BB, a substance that creates a more conducive environment for recovery at the injured area, it may provide an effective dual treatment approach. "We can integrate both methods — adjusting the internal characteristics of mature nerve cells through medication, along with our current strategy of modifying the non-nerve cell surroundings," explained Sun.
The Road Ahead
Although these findings are encouraging, some uncertainties still persist. Researchers aim to determine the optimal moment to administer PDGF-BB following an injury. Additionally, they seek to identify the appropriate dose and investigate if a sustained-release formulation might yield improved outcomes. As pericytes require time to arrive at the injured area, there could be a specific timeframe during which the therapy is most beneficial.
Notably, the therapy required just one administration to produce significant effects in mice. However, humans may require a more sustained or recurring course of treatment. Further research will investigate these aspects. Currently, it is evident that this single protein can convert cells that previously hindered recovery into allies in the healing process. Through altering the behavior of pericytes, researchers have discovered a method to restore the structural integrity of an injured spinal cord.
So far, PDGF-BB has emerged as an unexpected champion in the ongoing battle to repair harm caused by spinal cord injuries—one cellular bridge at a time.
Research results can be found online in the journal Molecular Therapy 00294-1?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS1525001625002941%3Fshowall%3Dtrue).
Note: The article mentioned above was provided by The Positive Aspect of Current Events .
Enjoy these types of uplifting tales? Obtain The Positive Aspect of Daily News' mailing list .

Posting Komentar untuk "Breakthrough Protein Unlocks Body’s Healing Power for Spinal Injuries"
Please Leave a wise comment, Thank you